Understanding Central Vision Loss in Older Adults – A UKMLA/PLAB Question Analysis
Decode Complex Exam Questions for UKMLA and PLAB Success
This article dissects a tricky question from the August 2024 PLAB 1 exam, focusing on a common yet challenging condition: age-related macular degeneration (AMD). As the leading cause of central vision loss in older adults, AMD tests clinical reasoning and diagnostic skills, making it a crucial topic for medical exams like the UKMLA, PLAB, and USMLE.
PLAB Exam Case Scenario: A 75-year-old man presents with difficulty recognizing faces and reading, which has gradually worsened over the past year. He reports that straight lines appear wavy. On examination, there is a loss of central vision in both eyes.
What is the most likely diagnosis?
- A) Glaucoma
- B) Diabetic retinopathy
- C) Age-related macular degeneration
- D) Cataracts
- E) Retinal detachment
Answer with an explanation is provided below.
Our content is updated to align with the MLA content map
〰️
Our content is updated to align with the MLA content map 〰️
The ultimate preparation tool for your PLAB or UKMLA exam
Were MedRevisions.com materials enough to pass the First PLAB exam that was based of the MLA content map?: Visit here to see what this doctor had to say
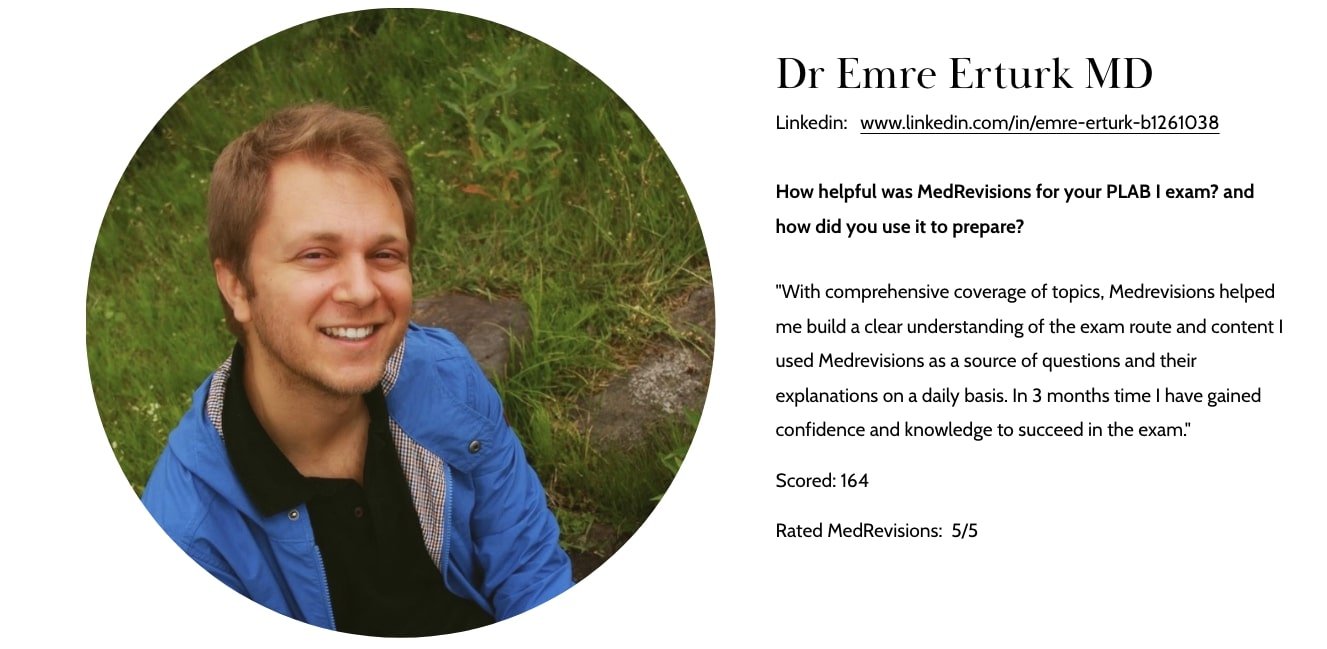
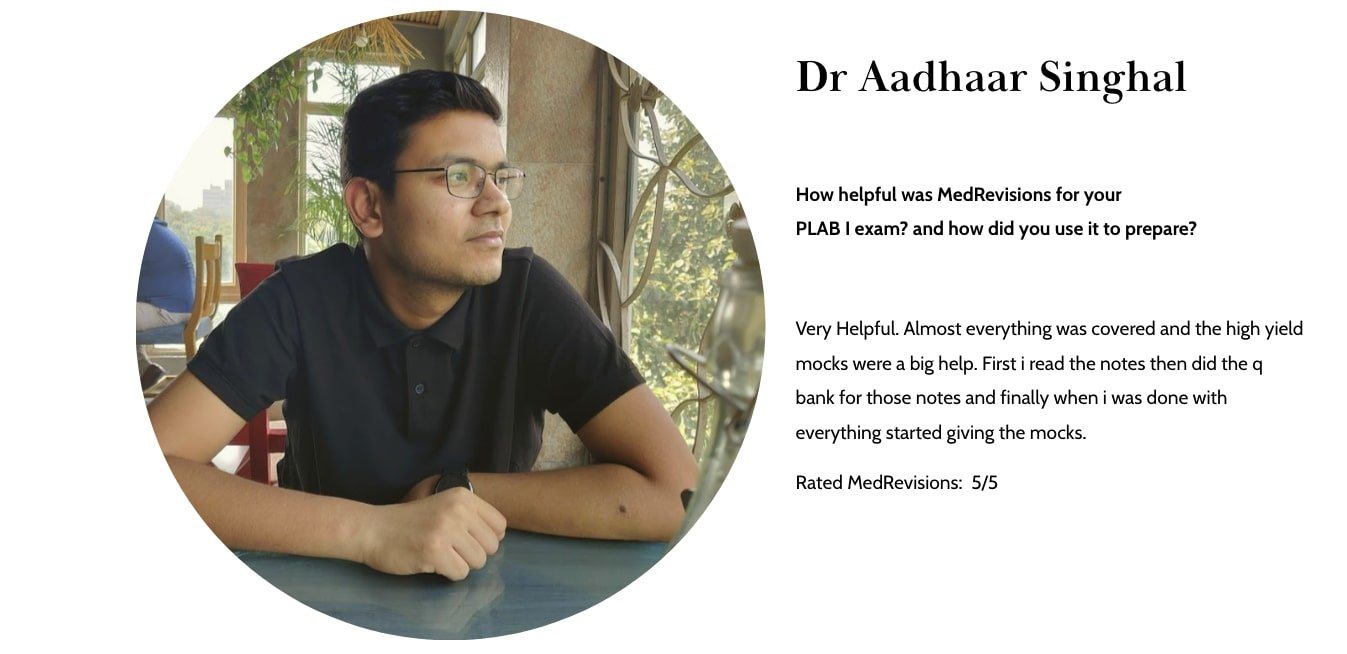
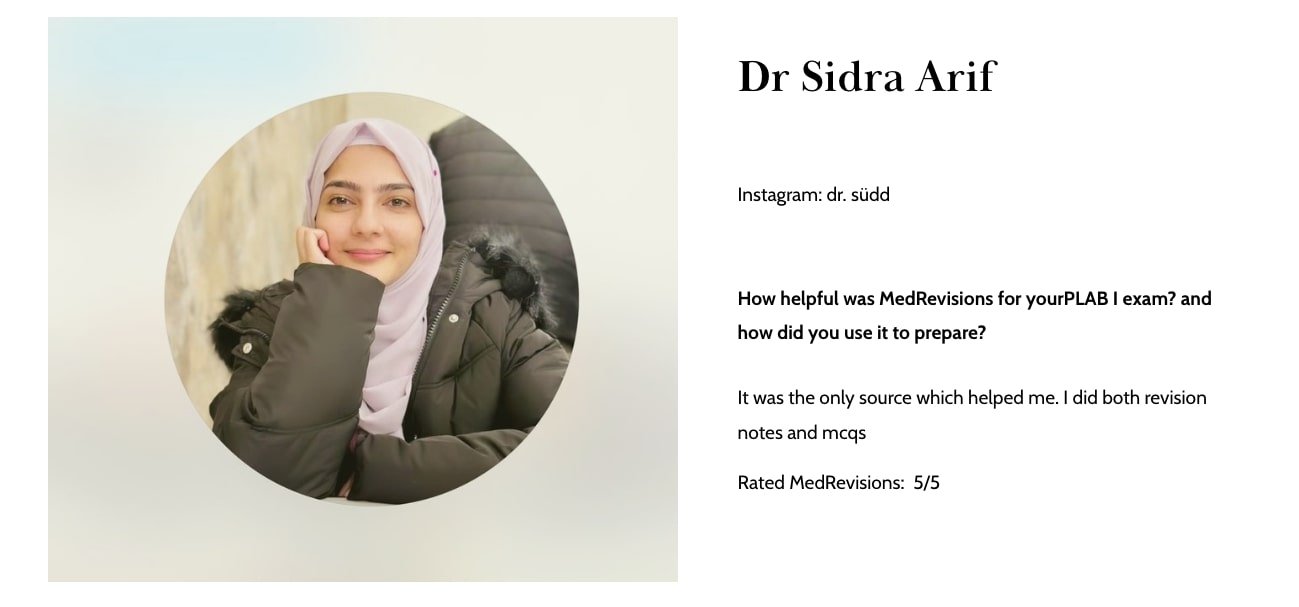
Past PLAB 1 candidates reviews about MedRevisions verified with results
Follow us on telegram for more free questions
Helpful Study groups for the PLAB or MLA exam
Find the 10% discount referral links in the groups
More about the UKMLA or PLAB exam:
Important update to the PLAB exam: Is the PLAB exam based on the MLA content map from August 2024 onward? Find out more about the change and how to prepare for it here.
Evolving Nature of PLAB 1 Exam Questions: Is the exam getting tougher? A Closer Look with examples
What Past PLAB 1 candidates say about us (with exam results)
Explanation of the above PLAB / UKMLA exam question
Correct Answer: C) Age-Related Macular Degeneration (AMD)
Why Age-Related Macular Degeneration (AMD) is the Most Likely Diagnosis
Symptoms Match AMD: AMD is the leading cause of central vision loss in older adults and is associated with difficulty reading and recognising faces due to the involvement of the macula.
Metamorphopsia: The symptom of wavy lines is characteristic of wet AMD, where fluid or blood accumulates under the retina, distorting vision.
Bilateral Presentation: AMD typically affects both eyes, though not necessarily symmetrically, which fits this patient’s findings.
Why Other Options are Less Likely:
A) Glaucoma: Glaucoma primarily causes peripheral vision loss, not central vision loss. It progresses silently and does not typically cause metamorphopsia or distorted vision.
B) Diabetic Retinopathy: Diabetic retinopathy causes vision loss due to retinal haemorrhages, macular oedema, or detachment, but it is usually associated with a history of diabetes. This is not mentioned in the scenario.
D) Cataracts: Cataracts cause blurred vision, glare, and difficulty seeing at night. However, they do not typically cause wavy lines or central vision loss, as seen in this case.
E) Retinal Detachment: Retinal detachment presents acutely with symptoms like a sudden curtain-like shadow, flashes of light, and floaters, which are not present here. It does not typically cause progressive central vision loss over a year.
Management and Follow-Up:
Confirm Diagnosis: Refer the patient to an ophthalmologist for further evaluation, including optical coherence tomography (OCT) and fundoscopy to confirm AMD and differentiate between the dry and wet types.
Treatment:
Dry AMD: Focuses on lifestyle modifications, such as smoking cessation, dietary supplements (e.g., antioxidants), and vision aids.
Wet AMD: Requires treatment with intravitreal anti-vascular endothelial growth factor (anti-VEGF) injections (e.g., ranibizumab or aflibercept) to reduce fluid accumulation and slow progression.
Monitoring: Regular follow-up with an ophthalmologist is necessary to monitor disease progression and response to treatment.
🎓 New Study Essential Mode For PLAB 1/UKMLA exam
For Focused, efficient, targeted learning for PLAB and UKMLA exam
This update gives you the freedom to prepare for your exam in a short time and cover the syllabus with around 1800+ questions and our updated notes. Then leverage the remaining 3000+ exam-style questions and solidify your concepts. Know how to use it from the link below and get access to the most updated and reliable exam-like materials. Learn more about the Study Essential Mode
Reference:
NICE Guidelines: Urinary Tract Infection in Children and Young People.
Remember: This blog post is for educational purposes only and should not be considered medical advice.
This is a high-yield exam PLAB 1/ UKMLA question-style question. At MedRevisions, We provide questions and not only explain the correct answer, we also explain the wrong answer so you will have a comprehensive understanding of the concepts that is commonly tested in the exam. On top of that, we also provide you PLAB 1 / UKMLA exam curated notes with no additional cost.
To discuss to more PLAB or UK-MLA exam questions, Join: PLAB 1 /UKMLA exam study group
At MedRevisions, we strive hard to provide the most up-to-date content available for PLAB Part 1. We constantly add exam-style questions derived from the most recent exam and also update the content to align with the latest NICE/CKS guidelines to ensure doctors pass PLAB Part 1 or UKMLA exam with ease in ONE attempt.
Past PLAB 1 candidates reviews about MedRevisions
How to use MedRevisions effectively for the PLAB 1 exam/ UKMLA exam preparation
Previous PLAB 1 or UKMLA exam guideline update
All MedRevisions recent updates
What we provide:
✅ 5000+ exam style questions
✅ Perfectly tailored exam style notes
✅ 30+ exam mocks
✅ Spaced repetition learning tool